Community Health Systems Inc. to Pay $98.15 Million to Resolve False Claims Act Allegations
The Justice Department announced that Community Health Systems Inc. (CHS), the nation’s largest operator of acute care hospitals, has agreed to pay $98.15 million to resolve multiple lawsuits alleging that the company knowingly billed government health care programs for inpatient services that should have been billed as outpatient or observation services. The settlement also resolves allegations that one of the company’s affiliated hospitals, Laredo Medical Center (LMC), improperly billed the Medicare program for certain inpatient procedures and for services rendered to patients referred in violation of the Physician Self-Referral Law, commonly known as the Stark Law. CHS is based in Franklin, Tennessee, and has 206 affiliated hospitals in 29 states.
“Charging the government for higher cost inpatient services that patients do not need wastes the country’s health care resources,” said Assistant Attorney General Stuart F. Delery for the Justice Department’s Civil Division. “In addition, providing physicians with financial incentives to refer patients compromises medical judgment and risks depriving patients of the most appropriate health care available. This department will continue its work to stop this type of abuse of the nation’s health care resources and to ensure patients receive the most appropriate care.”
The United States alleged that from 2005 through 2010, CHS engaged in a deliberate corporate-driven scheme to increase inpatient admissions of Medicare, Medicaid and the Department of Defense’s (DOD) TRICARE program beneficiaries over the age of 65 who originally presented to the emergency departments at 119 CHS hospitals. The government further alleged that the inpatient admission of these beneficiaries was not medically necessary, and that the care needed by, and provided to, these beneficiaries should have been provided in a less costly outpatient or observation setting. CHS agreed to pay $89.15 million to resolve these allegations. The settlement does not include hospitals that CHS acquired from Health Management Associates (HMA) in January 2014.
In addition, the government alleged that from 2005 through 2010, one of CHS’s affiliated hospitals, LMC in Laredo, Texas, presented false claims to the Medicare program for certain cardiac and hemodialysis procedures performed on a higher cost inpatient basis that should have been performed on a lower cost outpatient basis. The government also alleged that from 2007 through 2012, LMC improperly billed Medicare for services referred to LMC by a physician who was offered a medical directorship at LMC, in violation of the Stark Law. The Stark Law prohibits a hospital from submitting claims for patient referrals made by a physician with whom the hospital has an improper financial relationship, and is intended to ensure that a physician’s medical judgment is not compromised by improper financial incentives, and is instead based on the best interests of the patient. CHS agreed to pay $9 million to resolve the allegations involving LMC.
“This is the largest False Claims Act settlement in this district and it reaffirms this office’s commitment to investigate and pursue health care fraud that compromises the integrity of our health care system,” said U.S. Attorney David Rivera for the Middle District of Tennessee. “This office is committed to ensuring that all companies billing government healthcare programs are responsible corporate citizens and that hospital providers do not engage in schemes to increase medically unnecessary in-patient admissions of government healthcare program beneficiaries in order to increase profits.”
“This settlement demonstrates our commitment to working with our law enforcement partners and with the Department of Justice to protect the integrity of our nation’s health care system,” said U.S. Attorney Kenneth Magidson of the Southern District of Texas. “Put simply, these types of fraudulent practices will not be tolerated and the investigation and resolution of such claims will continue to be a high priority of this office.”
“Health care providers should make treatment decisions based on patients’ medical needs, not profit margins,” said U.S. Attorney Anne M. Tompkins for the Western District of North Carolina. “We will not allow this type of misconduct to compromise the integrity of our health care system.”
As part of agreement, CHS entered into a Corporate Integrity Agreement with the U.S. Department of Health and Human Services - Office of Inspector General (HHS-OIG), requiring the company to engage in significant compliance efforts over the next five years. Under the agreement, CHS is required to retain independent review organizations to review the accuracy of the company’s claims for inpatient services furnished to federal health care program beneficiaries.
“In an effort to ensure the company’s fraudulent past is not its future, CHS agreed to a rigorous multi-year Corporate Integrity Agreement requiring that the company commit to compliance with the law,” said Inspector General Daniel R. Levinson, of the U.S. Department of Health and Human Services. “The dedicated work of OIG’s investigators, auditors, and attorneys, in concert with our law enforcement partners, has again resulted in the recovery of taxpayer dollars and better protection against fraud in the future.”
Source: U.S. Department of Justice
- 309 reads
Human Rights
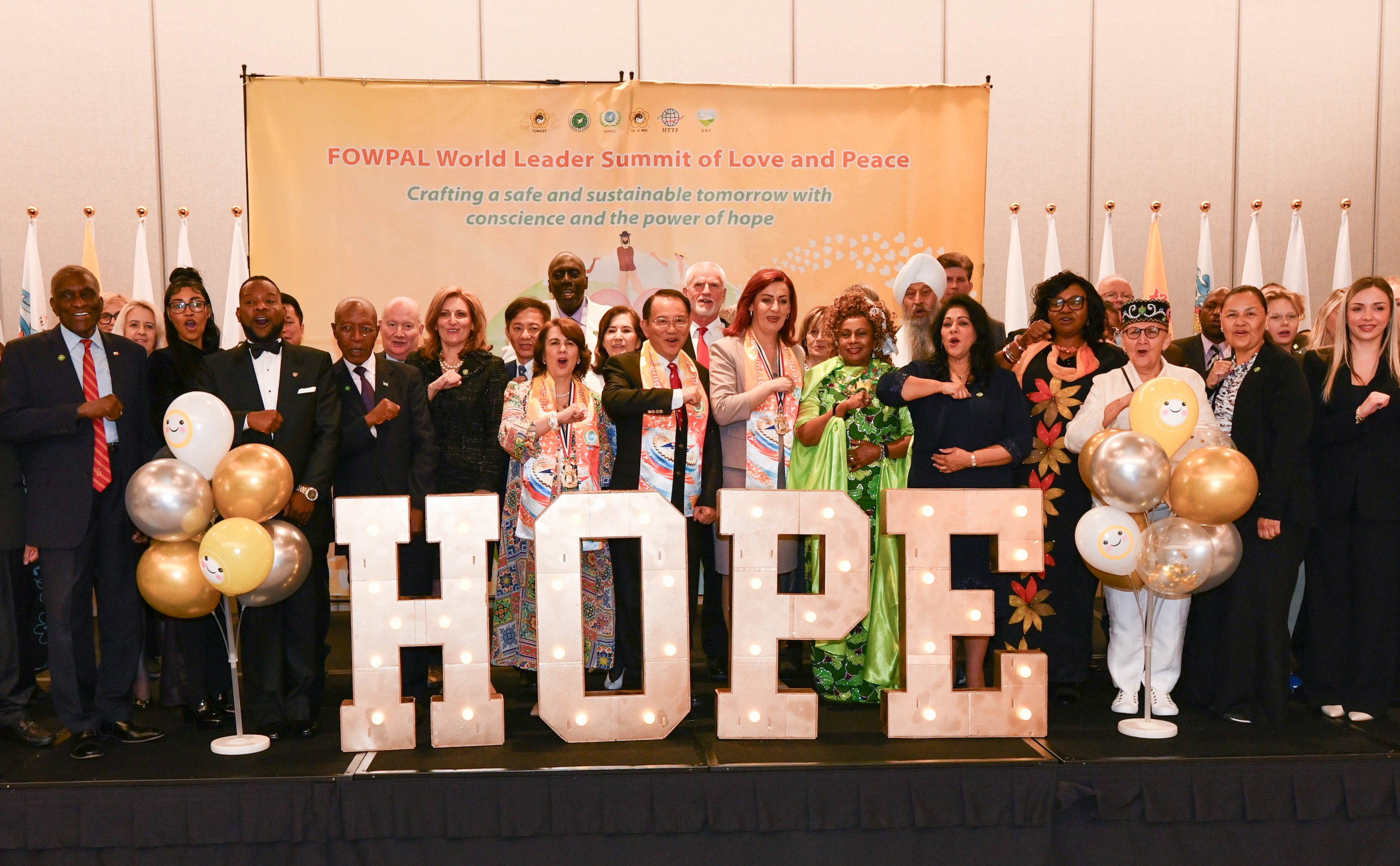
Ringing FOWPAL’s Peace Bell for the World:Nobel Peace Prize Laureates’ Visions and Actions

Protecting the World’s Cultural Diversity for a Sustainable Future

The Peace Bell Resonates at the 27th Eurasian Economic Summit

Declaration of World Day of the Power of Hope Endorsed by People in 158 Nations

Puppet Show I International Friendship Day 2020