Rights Risks to Older People in COVID-19 Response
Combat Ageism; Ensure Access to Health Care, Services
Governments should respect the rights of older people in their response to the COVID-19 epidemic, Human Rights Watch said on April 06, 2020.
Available evidence has shown that older people are more likely to experience serious and life-threatening complications from COVID-19 infection. Older people also face a heightened risk of infection if they live in institutions like nursing homes and may face severe social isolation if they remain at home. They face further risks to their health and rights in detention, and with reliance on humanitarian aid.
“Older people are disproportionately affected by COVID-19, and many governments are racing to respond,” said Bethany Brown, researcher on older people’s rights at Human Rights Watch. “But older people face risks to their rights as well if governments do not take their specific experiences into account and do not actively combat age discrimination.”
More than 95 percent of the people who have reportedly died of COVID-19 in Europe were over age 60. The US Centers for Disease Control and Prevention reported that from February 12 to March 16, 2020, COVID-19 fatality in the United States was highest in people over 85, followed by people ages 65 to 84.
In addition to the greater risk of severe illness and death from the virus, discriminatory attitudes and actions threaten older people’s rights. A United Kingdom newspaper opinion piece about the economic impact of the coronavirus said that the death of older people could actually be beneficial by “culling elderly dependents.” In a March 22 interview, Ukraine’s former health minister said people over 65 are already “corpses” and the government should focus its COVID-19 efforts on people “who are still alive.”
The Texas lieutenant governor, Dan Patrick, suggested that older people might be willing to sacrifice themselves to benefit the economy: “My message is that let’s get back to work,” Patrick, 69, said on a national television program on March 23. “Let’s get back to living. Let’s be smart about it, and those of us who are 70-plus, we’ll take care of ourselves, but don’t sacrifice the country.”
Some governments have placed severe restrictions on freedom of movement based on age, forcing older people to remain confined in their homes or face fines or other penalties.
As one example, in Bosnia and Herzegovina, for several weeks people over 65 were not allowed to go outside, with no exceptions for grocery shopping, pharmacy visits, or even taking out the garbage. Over 200 older people were fined. On April 3, the government revised the rule to allow older people to go out between 7 a.m. and noon, Monday through Friday.
Older people who find themselves unexpectedly alone without control over their circumstances are at particular risk for a variety of severe, even life-threatening, physical and mental health conditions, including cognitive decline. Restrictions on freedom of movement should be proportionate and not based exclusively on age.
Governments should address the risks of social isolation while ensuring health needs during “social distancing,” Human Rights Watch said.
COVID-19, like other infectious diseases, poses a higher risk to populations that live in close proximity. This risk is particularly acute in nursing or aged care facilities, where the virus can spread rapidly and has already resulted in many deaths. About 1.5 million older people live in nursing facilities in the US, excluding assisted living facilities and other settings creating close proximity.
Twenty-three people died in an outbreak at a facility in Washington State in February and March, and the US Centers for Disease Control reported 400 more cases in facilities as of April 1. On March 31, health authorities in the Grand Est region of France reported 570 deaths of older people in nursing facilities.
Older people often end up in nursing homes due to governments’ failure to provide sufficient social services for people to live independently in the community, policies that have put millions at added risk of contracting the virus because of their institutionalization. Governments should ensure continuity of community-based services so that people do not end up in institutions in the absence of other options.
The UK government, instead of improving social care provisions for older people, especially in England, at this time, has instead suspended requirements for social care assessments and services arrangements. Some emergency rules, such as restrictions on public gathering and transport, may be justified amid the continuing spread of the disease. But relaxing rules for assessments and other aspects of social care creates the potential for violations of fundamental human rights.
The US government, to try to counter the COVID-19 risks facing older people in nursing facilities, announced a “no visitors” policy. Some Australian facilities are following this lead beyond the Australian government’s public health guidance, which limits visitors to a maximum of two people per visit, requires the visits to be of short duration, and has guidelines on hygiene and physical distancing.
Nursing home policies should balance protecting older and at-risk residents with their needs for family and connection as well as the important oversight that visitors provide. A more balanced approach to keeping residents and nursing facility staff safe could restrict visitors who are sick, as many facilities already do; strictly supervise visitors’ handwashing and wearing of masks, and social distancing; and have a dedicated room for visiting.
Many national health systems are overwhelmed by the number of patients experiencing serious complications from COVID-19. Age should not be a primary criterion for denying treatment. Governments should issue clear policies to guide medical personnel in decisions about allocating resources and monitor for discrimination in accessing medical services for all high-risk groups, including older people. Governments should also recognize and respond to intersecting types of discrimination. For example, the older LGBT population has higher rates of HIV and cancer, which can lead to compromised immune systems, increasing vulnerability to severe complications with COVID-19 infection.
Thousands of older people live in refugee and displaced people’s camps, where they face health risks from crowded conditions and limited access to health and hygiene supplies. Governments should ensure that older refugees and displaced older people get health care, including access to national health systems and hospitals, regardless of legal status. In camps, older people should also have access to the shelter, water, and sanitation facilities they need to maintain their health, with specific attention to accessible handwashing support.
Older people should be given particular consideration for release from prisons, jails, and detention centers. In the US, for example, older men and women are the fastest growing group in US prisons, due to lengthy sentences, and prison officials already have difficulty providing them appropriate medical care.
“Governments should not respond to threats to older people’s health with threats to their rights,” Brown said. “We are all at risk if government responses to this epidemic reinforce ageist attitudes and ignore older people’s equal rights.”
Source:Human Rights Watch
- 266 reads
Human Rights
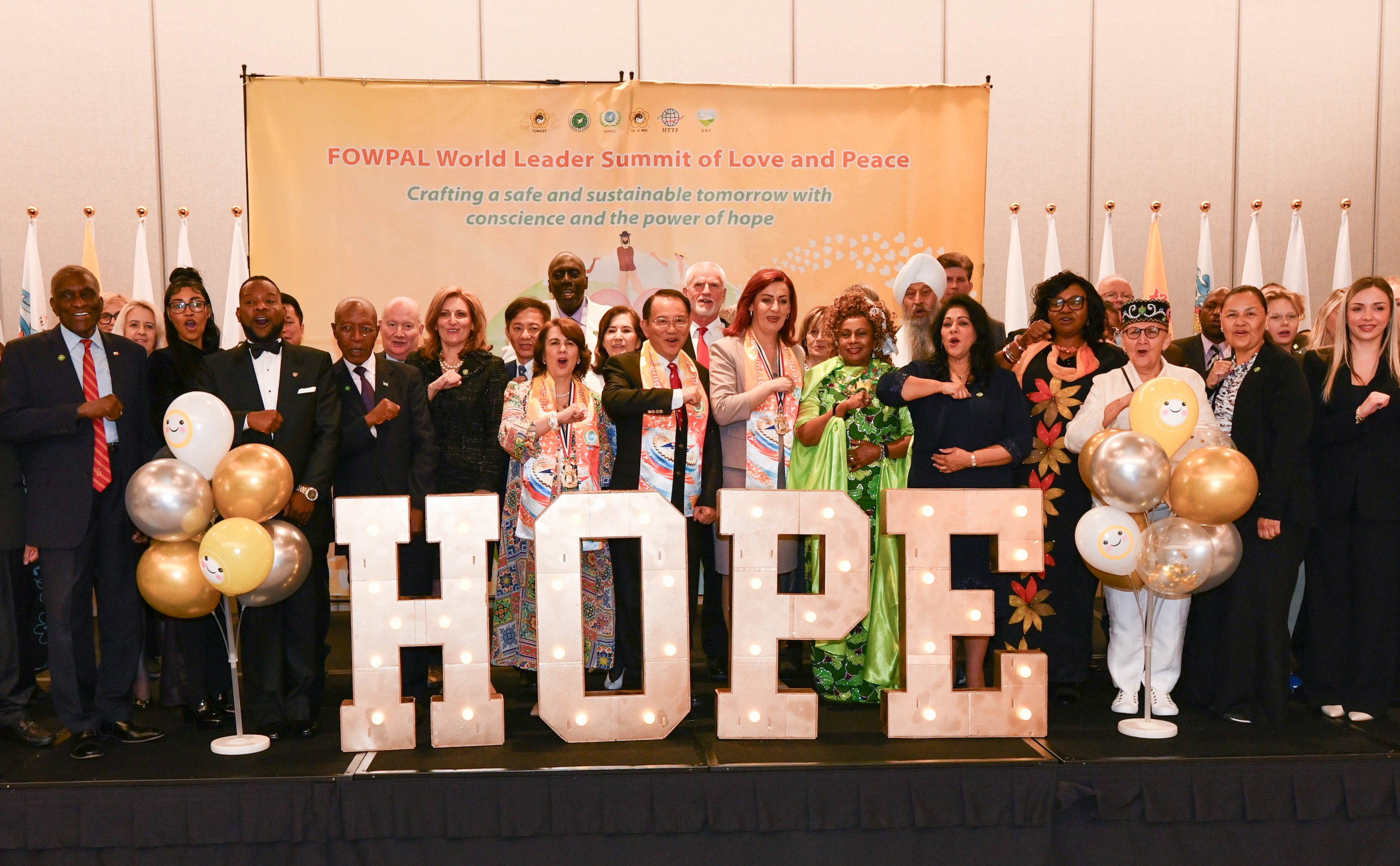
Ringing FOWPAL’s Peace Bell for the World:Nobel Peace Prize Laureates’ Visions and Actions

Protecting the World’s Cultural Diversity for a Sustainable Future

The Peace Bell Resonates at the 27th Eurasian Economic Summit

Declaration of World Day of the Power of Hope Endorsed by People in 158 Nations

Puppet Show I International Friendship Day 2020