Preventive treatment reduces diabetic retinopathy complications
In a clinical trial, early treatment with anti-vascular endothelial growth factor (VEGF) injections slowed diabetic retinopathy, a complication of diabetes that causes damage to the blood vessels of the light-sensitive tissue in the retina. However, two years into the four-year study, the early treatment’s effect on vision – including changes in visual acuity and vision loss - was similar to standard treatment, which usually begins only after the onset of late disease. The intermediate findings from the DRCR Retina Network (DRCR.net) published on March 31.

A doctor examines a patient’s eyes
“While it is possible that preventive injections of anti-VEGF drugs may help protect vision in the longer-term, we saw no effect on vision at two years,” said Raj Maturi, M.D., Indiana University, Indianapolis, the protocol chair for the study. “These two-year results suggest that close monitoring and routine treatment when complications develop are key to preventing vision loss from diabetic retinopathy.”
An estimated 30 million Americans have diabetes, which can cause blood vessel abnormalities, including the growth of new blood vessels in the eye. In the early stages of diabetic retinopathy, called non-proliferative diabetic retinopathy, changes in the eye’s blood vessels are visible to clinicians but generally do not affect sight. In the advanced stages, people can develop proliferative diabetic retinopathy, where retinal blood vessels grow abnormally, and/or diabetic macular edema, where fluid leaks out of the retinal blood vessels. Both can lead to vision loss and blindness. Treatment, such as with anti-VEGF drugs, can slow or prevent vision loss in people with proliferative diabetic retinopathy or diabetic macular edema, if treatment occurs promptly.
In this study, participants with non-proliferative diabetic retinopathy were randomly assigned at baseline to receive either injections of Eylea (aflibercept) or a sham injection. They were examined at one, two, and four months, and then every four months for two years, receiving Eylea or sham injection at each visit. The researchers tracked their visual acuity and the severity of their diabetic retinopathy. If disease progressed, regardless of whether they were in the treatment or sham group, participants were given Eylea more frequently as is given in standard practice. If their condition did not improve with additional anti-VEGF treatment, participants could be given treatments such as laser photocoagulation or surgery if necessary.
The study included 328 participants (399 eyes). In two years, the rate of proliferative diabetic retinopathy development was 33% in the control group, compared with 14% in the treatment group. Likewise, the rate of development of diabetic macular edema affecting vision was 15% in the control group, compared with 4% in the treatment group. However, loss of visual acuity was essentially the same between the two groups at two years, suggesting that standard treatment at the appearance of proliferative diabetic retinopathy or diabetic macular edema affecting vision is sufficient to prevent further vision loss at this time point.
“We have a really good treatment for these diseases, so we can manage vision complications that may arise as disease progresses for many eyes,” said Adam Glassman, Jaeb Center for Health Research, Tampa, Florida, director of the DRCR.net coordinating center. “When evaluating new preventative treatment strategies, it is important to compare them directly to the standard treatment after disease worsens, as we have done in this study.”
“Although we did not see any difference in visual outcomes at two years, the four-year follow-up is going to be very important,” said Jennifer Sun, M.D., M.P.H., Joslin Diabetes Center, Harvard Medical School, Boston, chair of Diabetes Initiatives for the Network. “We look toward the four-year data to see whether reducing rates of diabetic retinopathy worsening will lead to long-term improvement in visual outcomes.”
Source: U.S. National Institutes of Health
- 378 reads
Human Rights
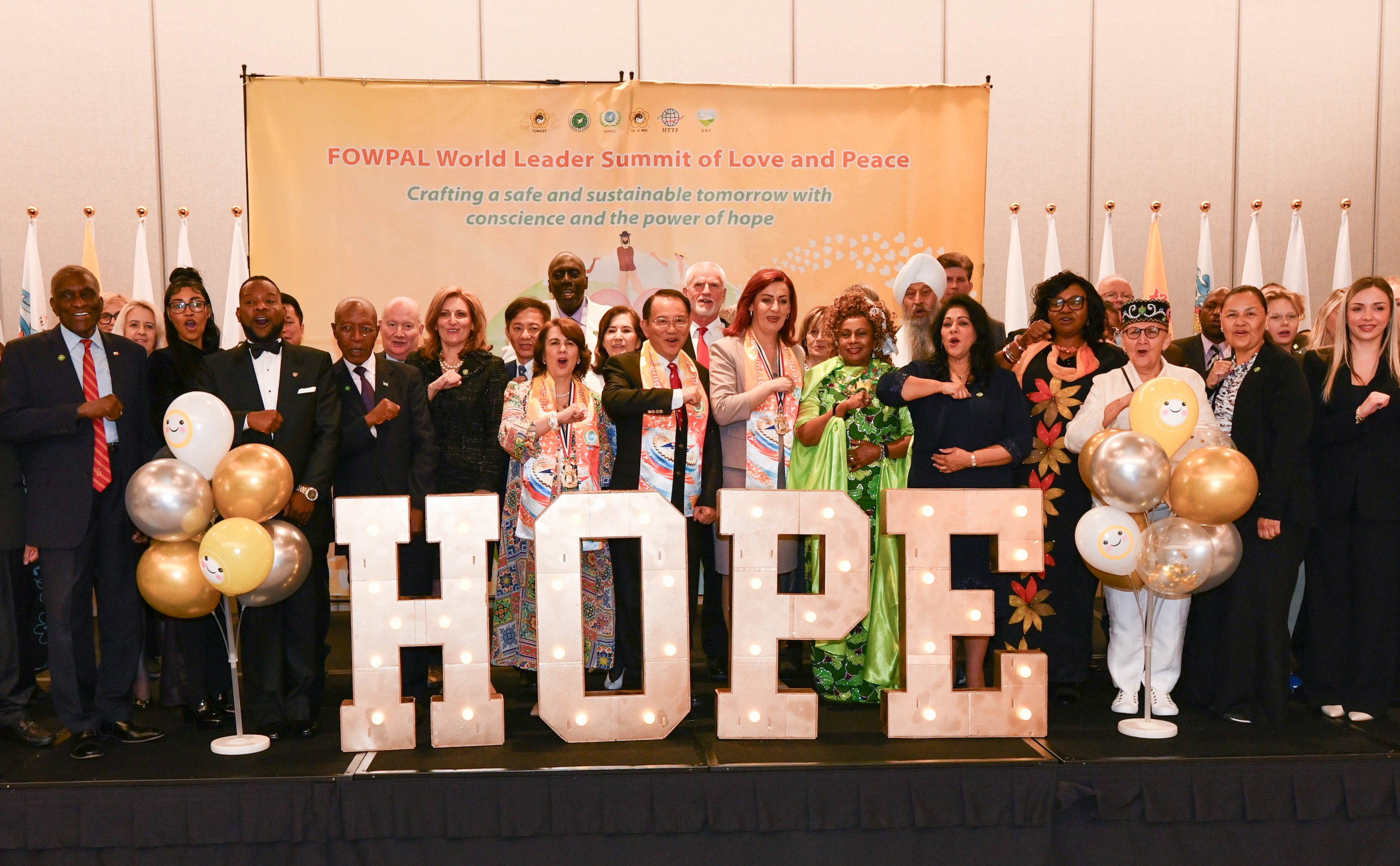
Fostering a More Humane World: The 28th Eurasian Economic Summi

Conscience, Hope, and Action: Keys to Global Peace and Sustainability

Ringing FOWPAL’s Peace Bell for the World:Nobel Peace Prize Laureates’ Visions and Actions

Protecting the World’s Cultural Diversity for a Sustainable Future

Puppet Show I International Friendship Day 2020