Scientists discover genetic and immunologic underpinnings of some cases of severe COVID-19
New findings by scientists at the National Institutes of Health and their collaborators help explain why some people with COVID-19 develop severe disease. The findings also may provide the first molecular explanation for why more men than women die from COVID-19.
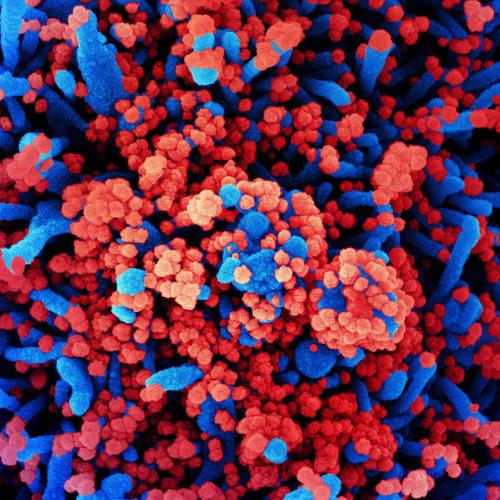
Colorized scanning electron micrograph of a cell (blue) heavily infected with SARS-CoV-2 virus particles (red), isolated from a patient sample. NIAID
The researchers found that more than 10% of people who develop severe COVID-19 have misguided antibodies―autoantibodies―that attack the immune system rather than the virus that causes the disease. Another 3.5% or more of people who develop severe COVID-19 carry a specific kind of genetic mutation that impacts immunity. Consequently, both groups lack effective immune responses that depend on type I interferon, a set of 17 proteins crucial for protecting cells and the body from viruses. Whether these proteins have been neutralized by autoantibodies or―because of a faulty gene―were produced in insufficient amounts or induced an inadequate antiviral response, their absence appears to be a commonality among a subgroup of people who suffer from life-threatening COVID-19 pneumonia.
The wide variation in the severity of disease caused by SARS-CoV-2, the virus behind COVID-19, has puzzled scientists and clinicians. SARS-CoV-2 can cause anything from a symptom-free infection to death, with many different outcomes in between. Since February 2020, Drs. Su and Casanova and their collaborators have enrolled thousands of COVID-19 patients to find out whether a genetic factor drives these disparate clinical outcomes.
The researchers discovered that among nearly 660 people with severe COVID-19, a significant number carried rare genetic variants in 13 genes known to be critical in the body’s defense against influenza virus, and more than 3.5% were completely missing a functioning gene. Further experiments showed that immune cells from those 3.5% did not produce any detectable type I interferons in response to SARS-CoV-2.
Examining nearly 1,000 patients with life-threatening COVID-19 pneumonia, the researchers also found that more than 10% had autoantibodies against interferons at the onset of their infection, and 95% of those patients were men. Biochemical experiments confirmed that the autoantibodies block the activity of interferon type I.
Source: U.S. National Institutes of Health
- 257 reads
Human Rights
Fostering a More Humane World: The 28th Eurasian Economic Summi

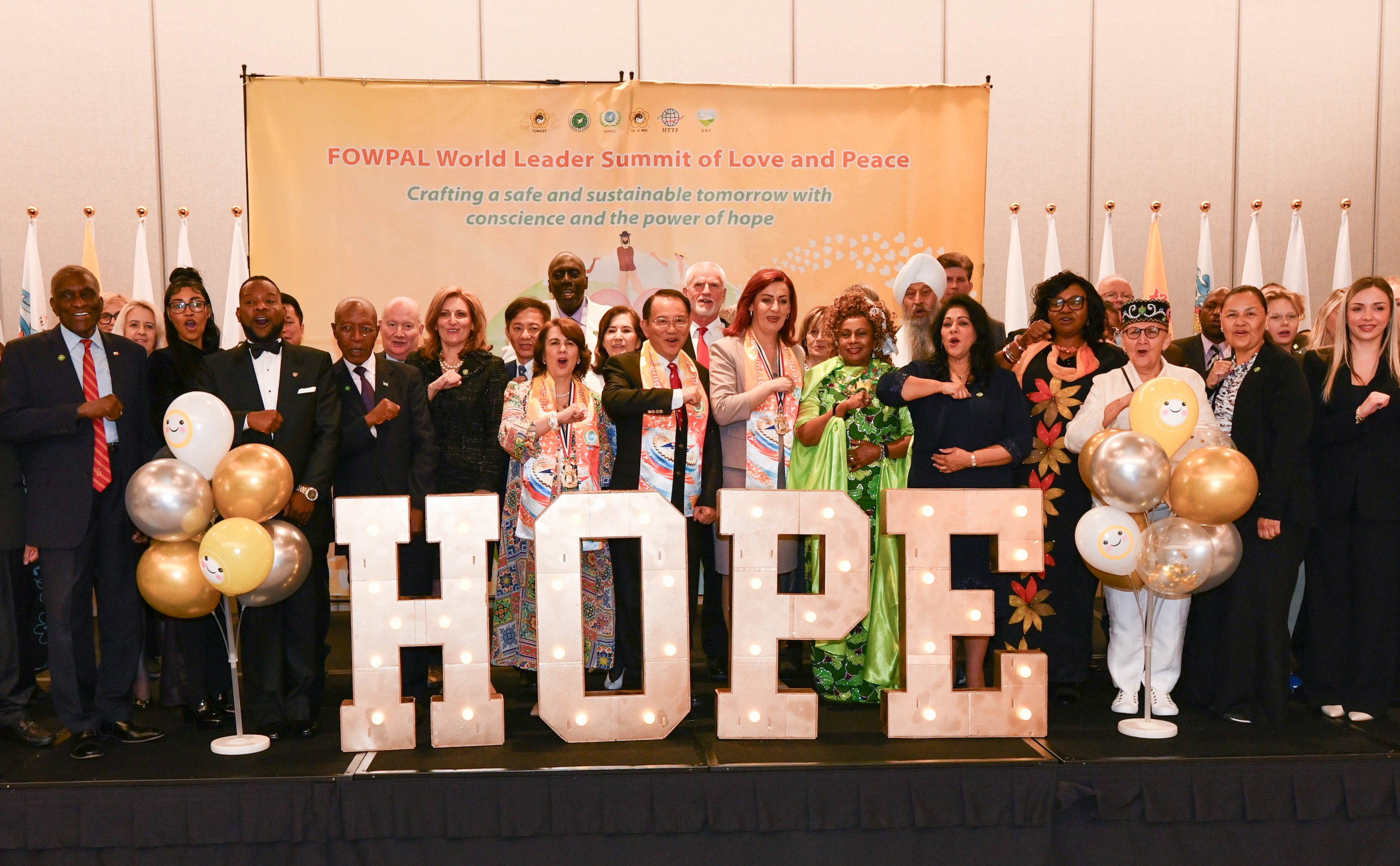
Conscience, Hope, and Action: Keys to Global Peace and Sustainability

Ringing FOWPAL’s Peace Bell for the World:Nobel Peace Prize Laureates’ Visions and Actions

Protecting the World’s Cultural Diversity for a Sustainable Future

Puppet Show I International Friendship Day 2020