AFRICA: The dilemma of discordance
Discordant couples, in which one partner is HIV-positive and the other HIV-negative, are increasingly common in African countries with high prevalence, but there is often little support to help them navigate the complexities that the virus adds to a relationship.
"The research and programming ... has largely had a biomedical focus. There is a black hole of information when it comes to the psycho-social aspects of HIV discordance," Kevin Moody, international coordinator of the Global Network of People living with HIV (GNP+), said at the International AIDS Conference in Vienna, Austria.
A 2008 study by GNP+ among discordant straight and gay couples in South Africa, Tanzania and the Ukraine found that they dealt with a raft of issues, from achieving intimacy to disclosure and dealing with discrimination.
"HIV-positive people are living longer, are healthier and are remaining sexually active," said Monique Tondoi, a social economist at Women Fighting AIDS in Kenya (WOFAK), who has been married for 20 years and living with HIV for 16.
"We need to know what choices are out there for HIV prevention, whether we can have children ... how to talk to our families about the diagnosis. You don't want to infect your partner, but you still want the intimacy, the love that comes with sex, so you need to know how to go about it."
The reproduction conundrum
Tondoi said that societal pressure on African women to have children was a particular concern.
Discordant couples are usually advised to use condoms to prevent HIV infection. Those wanting to conceive are sometimes encouraged to use assisted reproductive methods such as in-vitro fertilization (IVF), which are often prohibitively expensive. In many cases, couples are not given enough information to make an informed decision.
Research suggests that antiretroviral (ARV) therapy can lower viral load (the amount of virus in the blood) to undetectable levels, so discordant couples can have unprotected sex during the fertile days of a woman's cycle with very low risk of the HIV-negative partner becoming infected.
However, until more data is available to back up such findings, said Moody, "We prefer to err on the side of caution and advise correct and consistent condom use.”
Other options for HIV prevention among discordant couples are non-penetrative sex and abstinence, but African women rarely have a say as to when they will have sex, and are often coerced into having unprotected sex that could put them or their partner at risk.
"I consider myself to be an empowered woman, but even I have to fight with my husband about using a condom - he hates it," Tondoi said. "So imagine a woman in the village; how is she to protect herself, or protect him?"
Couples counselling
"Some of the reasons couples who are aware of their discordance might have unprotected sex are logistics, such as obtaining and ensuring you have a condom nearby," said Kristin Dunkle, lead author of a study on HIV transmission in marriage in Rwanda and Zambia, which recommends promoting voluntary counselling and testing for discordant couples.
After counselling, women in the study were able to strategically position condoms around the house so that if their husbands returned home drunk, they were quickly able to reach for one and use it.
Another study suggested that couples counselling would be particularly important as new treatment options had the potential to decrease concerns about HIV transmission.
Tondoi noted that there was a need for HIV-prevention awareness among discordant couples, and for policies, services and research geared to their situation.
"These days it's a long time between an HIV-positive test and getting to the AIDS stage of infection," said Major Rubaramira Ruranga, an HIV-positive AIDS activist from Uganda. "We need options; we need research and education to get through life."
Source:IRIN PlusNews
- 716 reads
Human Rights
Fostering a More Humane World: The 28th Eurasian Economic Summi

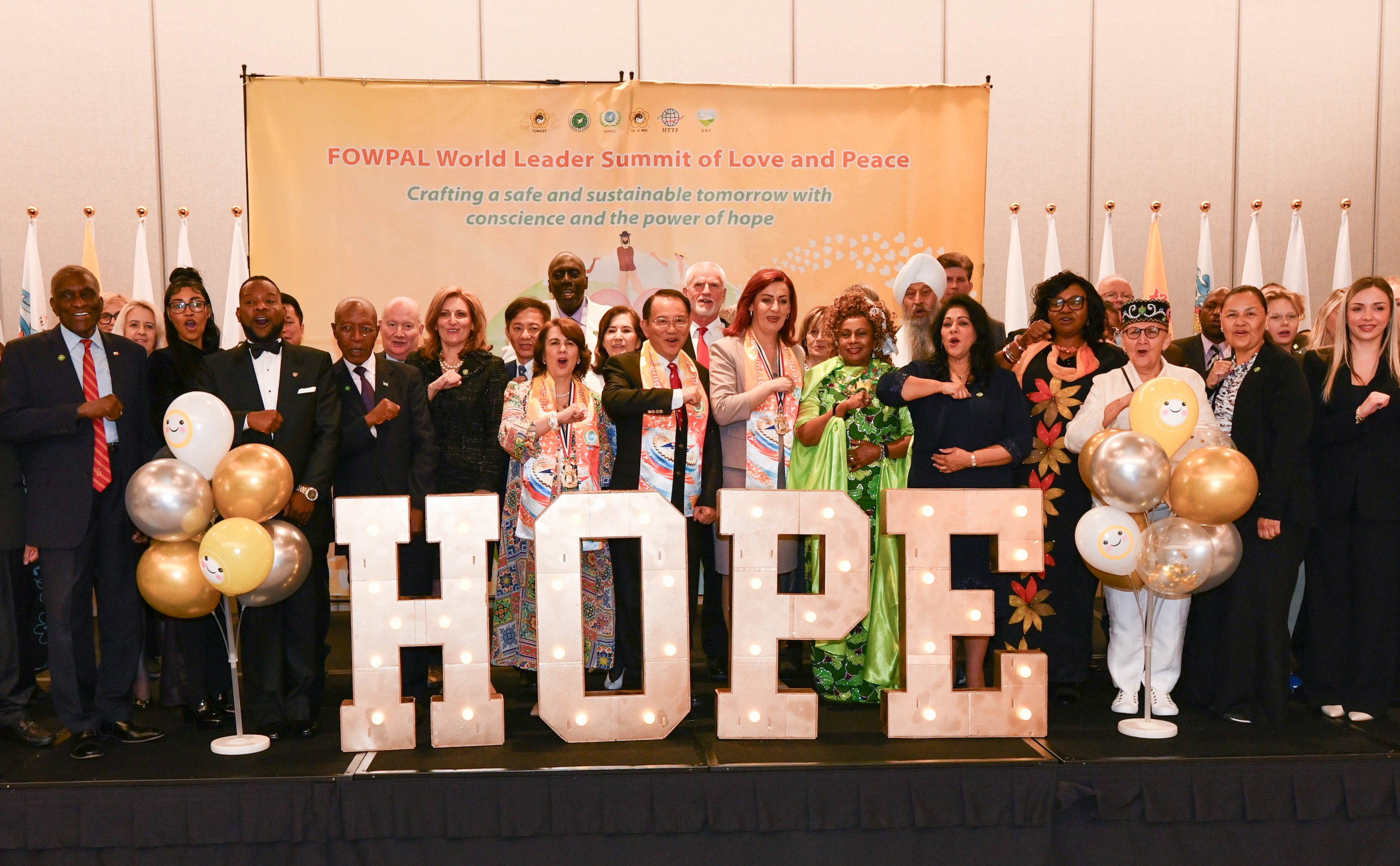
Conscience, Hope, and Action: Keys to Global Peace and Sustainability

Ringing FOWPAL’s Peace Bell for the World:Nobel Peace Prize Laureates’ Visions and Actions

Protecting the World’s Cultural Diversity for a Sustainable Future

Puppet Show I International Friendship Day 2020