Rehabilitation helps prevent depression from age-related vision loss
NIH-funded study brought together eye care and mental health professionals
Depression is a common risk for people who have lost their vision from age-related macular degeneration (AMD), but a new study shows that a type of rehabilitation therapy can cut this risk in half. The study was funded by the National Eye Institute (NEI), part of the National Institutes of Health.

An occupational therapist at Thomas Jefferson University works with a patient who has low vision.
“The results emphasize the high risk of depression from AMD, and the benefits of multi-disciplinary treatment that bridges primary eye care, psychiatry, psychology, and rehabilitation,” said expert.
AMD is a leading cause of vision loss in the United States. About 2 million Americans age 50 and over have vision loss from AMD, and about 8 million have an earlier stage of the disease, with or without vision loss. AMD causes damage to the macula, a spot near the center of the retina that is needed for sharp, straight-ahead vision. It can affect one eye or both, which is called bilateral AMD. As the disease progresses, it can cause a growing blurred area near the center of vision, and lead to difficulty with everyday activities, including the ability to drive, read, write, watch television, cook, and do housework.
Activities that used to be fun and fulfilling may begin to seem burdensome or even impossible. With loss of the ability to drive and navigate unfamiliar places, it becomes easier to stay at home than to see friends or meet new people. All of this can take a toll on mental health, and past studies have found that as many as one-third of people with bilateral AMD develop clinical depression.
“The depression is a response to disability, so we reasoned an effective treatment would be to reduce the disability through rehabilitation,” expert said. In the Low Vision Depression Prevention Trial (VITAL), who led a team of psychologists, ophthalmologists, optometrists, and occupational therapists to test an approach called behavior activation.
“Behavior activation involves helping people to focus on activities they enjoy, to recognize that loss of those activities can lead to depression, and to re-engage in those activities,” said expert. Helping people maintain an active social life is an important part of the approach.
The trial recruited 188 participants with bilateral AMD from an ophthalmology practice affiliated with Wills Eye Hospital in Philadelphia.
The participants were 84 years of age on average, 70 percent were women, and 50 percent lived alone. All had a best-corrected vision of less than 20/70. (A person with 20/70 vision sees an object from 20 feet away as clearly as a person with normal vision sees it at 70 feet away.) Each participant had mild depressive symptoms and was at risk for developing clinical depression, based on a nine-item depression subtest of the Patient Health Questionnaire, or PHQ-9.
During the trial, the participants had two visits with an optometrist, during which they were prescribed low-vision devices such as handheld magnifiers. After those initial visits, the participants were randomly split into two groups.
One group received behavior activation from an occupational therapist specially trained in the approach. The occupational therapist worked with participants to guide them on using the low-vision devices, to make changes around the home (such as using brighter lights and high-contrast tape), to increase their social activities, and to help them set personal goals and break these down into manageable steps.
“Blending the behavior activation with low-vision rehabilitation was straightforward and natural,” said expert. “Occupational therapy helps people regain valued activities in their daily lives, and behavior activation capitalizes on this through formal goal setting and reinforcement of progress.”
The second group of participants served as a control group. They talked about their difficulties to a therapist, but did not receive behavior activation or low-vision occupational therapy. Both groups had six one-hour therapy sessions in their homes over a two-month period. All participants were allowed to take antidepressants, but less than 10 percent did so. All received medical management of AMD as prescribed by their primary eye care providers.
By four months, 12 participants in the control group and seven participants in the behavior activation group had withdrawn from the trial or passed away. Of the remaining 169 participants, 18 (23.4 percent) in the control group and 11 (12.6 percent) in the behavior activation group developed clinical depression, based on retesting with the PHQ-9. Behavior activation had the most benefit for participants with the worst vision (less than 20/100), reducing the risk of depression by about 60 percent compared to controls. When the data were adjusted for vision status, physical health and baseline PHQ-9 score, behavior activation reduced the risk of depression by 50 percent compared to the control treatment.
AMD is typically diagnosed and treated in primary eye care settings, where there is no defined standard of care for depression. This study was a unique and compelling effort to address that issue by strengthening teamwork between eye care professionals and mental health professionals.
Expert hopes the study will serve as a model for similar approaches to preventing and treating depression in AMD. When approved by a physician, occupational therapy is reimbursable through Medicare.
“Stronger links between primary eye care and mental health care workers would be needed to make behavior activation more widely available for AMD patients,” expert said. Specialized instruction would also be needed for occupational therapists, who are not typically trained in behavior activation.
“We built this to be an affordable treatment. Now we would like to see it become accessible,” expert said. The study is continuing to follow participants to see if the benefits of treatment are maintained out to one year.
Source: U.S. National Institutes of Health
- 358 reads
Human Rights
Fostering a More Humane World: The 28th Eurasian Economic Summi

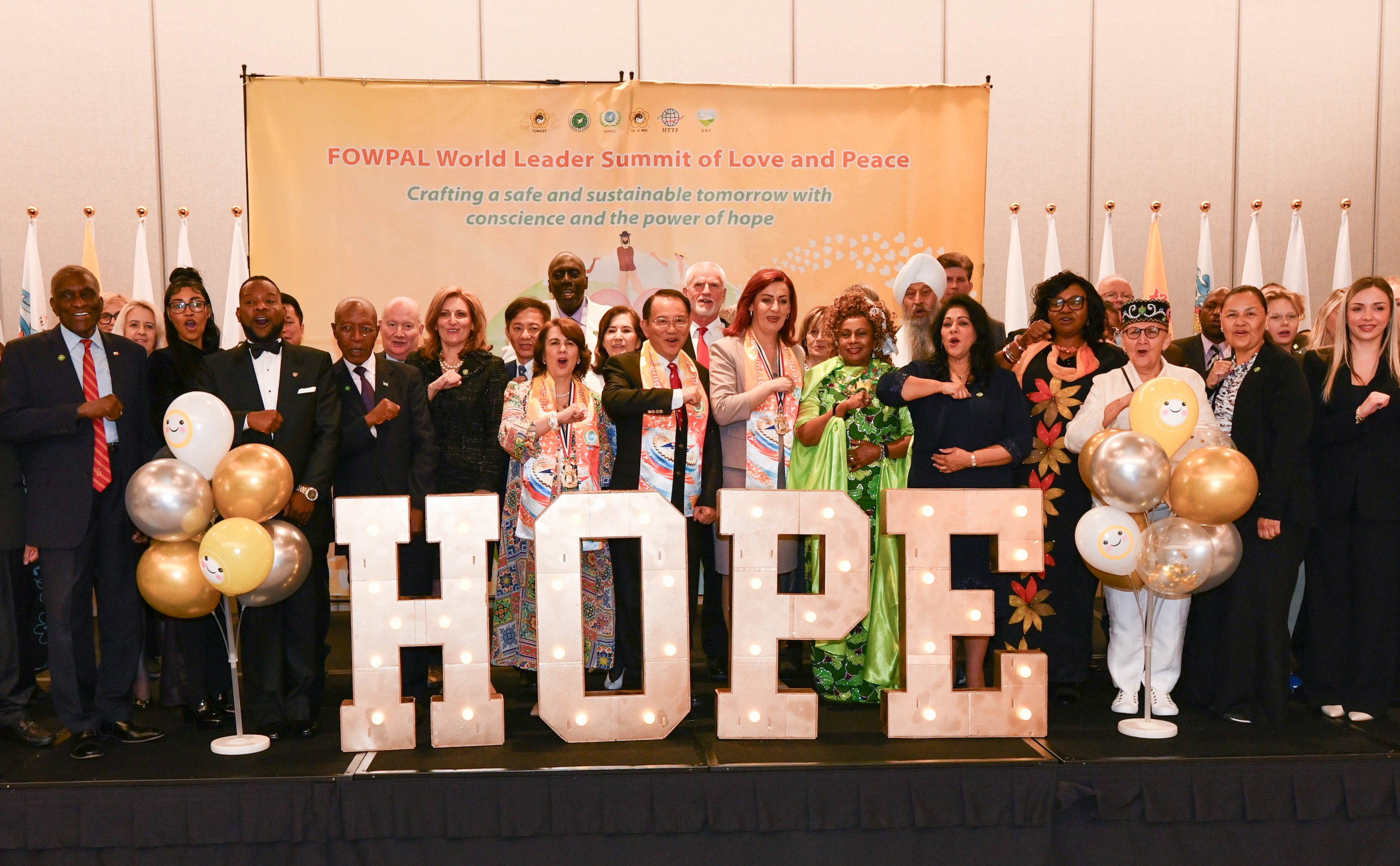
Conscience, Hope, and Action: Keys to Global Peace and Sustainability

Ringing FOWPAL’s Peace Bell for the World:Nobel Peace Prize Laureates’ Visions and Actions

Protecting the World’s Cultural Diversity for a Sustainable Future

Puppet Show I International Friendship Day 2020