Diabetes Tied to Higher Risk of Pancreatic Cancer in Study
But it's not always clear which disease comes first, researchers say.
People with diabetes have double the risk of pancreatic cancer compared to people who don't have diabetes, according to a new analysis of 88 previous studies.

Diabetes has been considered a risk factor for pancreatic cancer, but what's not clear is which condition comes first. This new analysis suggests that at least for some people, pancreatic cancer might be responsible for diabetes.
Experts note, however, that the overall risk for pancreatic cancer remains low among people with diabetes.
The study demonstrated that there is an overall two-fold increased risk of pancreatic cancer in patients with diabetes mellitus.
Diabetes mellitus includes type 1 and type 2 diabetes.
The study also demonstrates that diabetes mellitus itself may be an early indicator of the development of pancreatic cancer in certain cases. "Patients with diabetes mellitus that were analyzed had a seven-fold increased risk of being diagnosed with pancreatic cancer within the first year of being diagnosed with diabetes.
Studies have demonstrated that pancreatic cancer can produce certain substances that influence the way the body handles insulin and blood sugar, resulting in diabetes. In some patients with pancreatic cancer and diabetes, the diabetes actually improves once the cancer is removed.
But there is a plausible biological connection for diabetes to influence the growth of pancreatic cancer, too.
It is thought that the chemical changes that occur in the body with type 2 diabetes can promote the growth of pancreas cells and also result in damage that leads to the development of pancreatic cancer. Type 1 diabetes is similarly thought to be a risk factor, but to a lesser extent.
A U.S. expert said the review results are not unexpected.
Clearly, there is a relationship between diabetes and pancreatic carcinoma, and it could go in either direction. Pancreatic cancer might cause diabetes or diabetes might cause pancreatic cancer.
The overall risk of pancreatic cancer is quite low, so this isn't something that should worry most people with diabetes.
The risk of developing pancreatic cancer overall remains very low, even in long-standing diabetic patients. These patients should not be alarmed. It is even possible that good blood sugar control may lessen the risks.
A major problem with pancreatic cancer, however, is that it's often diagnosed at a very late stage. Overall five-year survival rates are less than 1 percent, and many patients diagnosed with late-stage pancreatic cancer don't survive more than four to six months after the diagnosis, according to background information included in the study.
Although the current review of past studies found an overall two-fold increased risk of pancreatic cancer in people with diabetes, that risk was highest soon after diagnosis. Within the first year after diagnosis, the risk of pancreatic cancer was nearly seven times higher than for someone without diabetes.
Although the risk stays elevated for a long time, after 10 years the risk of pancreatic cancer for someone with diabetes is just 36 percent higher than for someone without diabetes.
This suggests a window of opportunity for diagnosing pancreatic cancer earlier than it is currently. Detection methods for pancreatic cancer may include CT scans, PET scans and endoscopy. Testing for pancreatic cancer is often expensive.
It would not be feasible to screen all people with diabetes. Patients over the age of 55 without significant risk factors for diabetes who develop diabetes out of the blue appear to be a potentially good initial screening target.
Ratner agreed that it wouldn't make sense to screen everyone newly diagnosed with diabetes for pancreatic cancer because so few would have it.
There are circumstances where it might make sense. Someone with a family history of pancreatic cancer or a history of chronic pancreatitis or someone who smokes already has an increased risk of pancreatic cancer.
If the onset of diabetes is associated with a loss of appetite and weight loss, that's not the typical onset of type 2 diabetes. Type 2 usually causes hunger and isn't associated with a loss of weight. If someone's risk is higher and the onset of diabetes isn't typical, that's someone who may warrant more substantive investigation.
Source: HealthDay News
- 341 reads
Human Rights
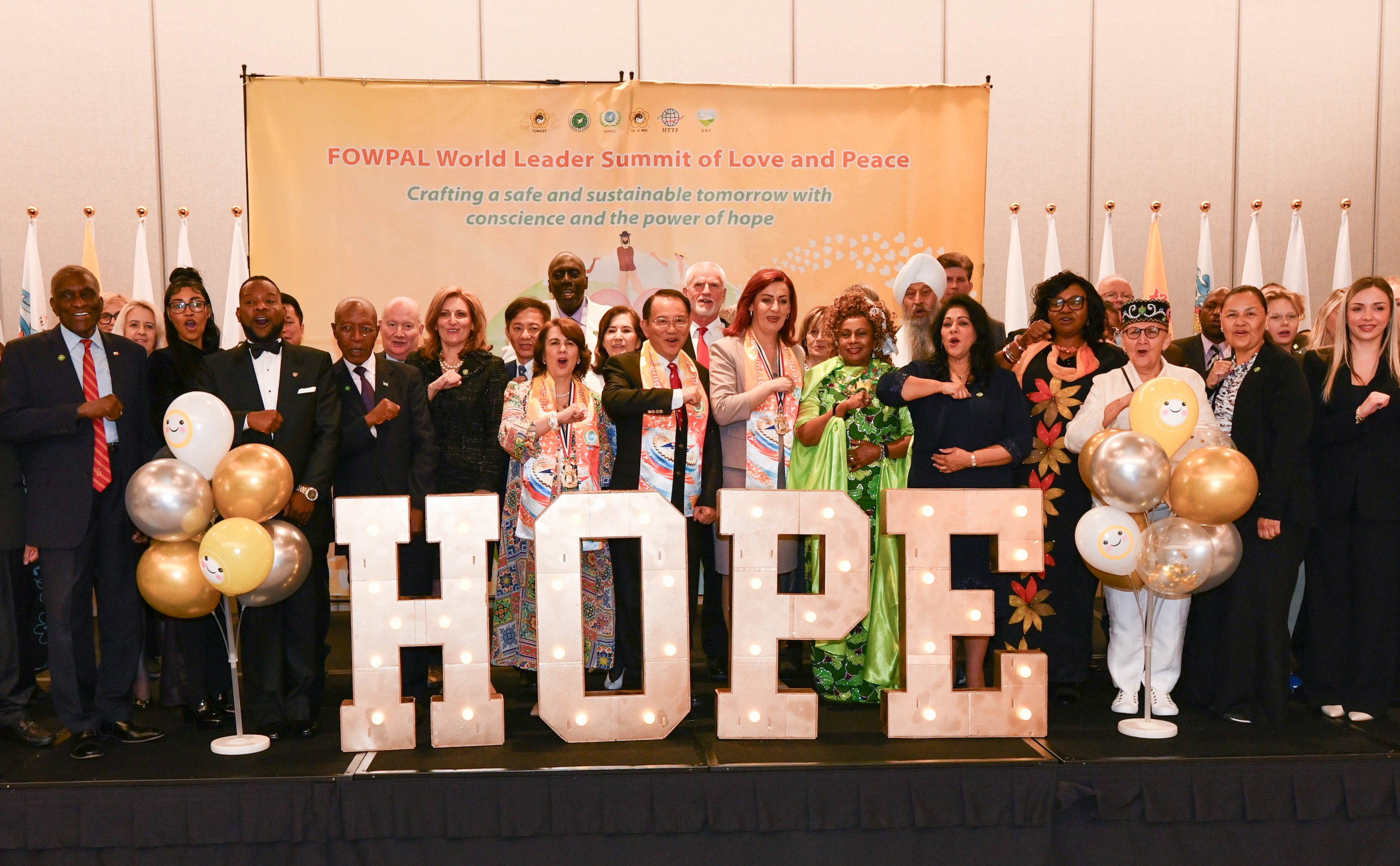
Fostering a More Humane World: The 28th Eurasian Economic Summi

Conscience, Hope, and Action: Keys to Global Peace and Sustainability

Ringing FOWPAL’s Peace Bell for the World:Nobel Peace Prize Laureates’ Visions and Actions

Protecting the World’s Cultural Diversity for a Sustainable Future

Puppet Show I International Friendship Day 2020